Cardiac Pacemaker
CARDIAC PACEMAKERS WHAT MY PATIENTS NEED TO KNOW BEFORE IMPLANT

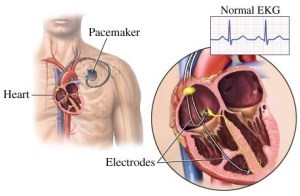
What is a Pacemaker?
A Pacemaker is a small device implanted under your skin, usually near the collarbone, to help control your heartbeat. It mimics the heart’s natural pacemaker, sending electrical signals to keep your heart beating regularly when its natural “battery” slows down or fails.
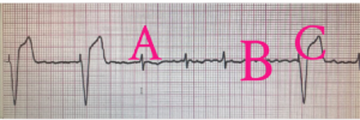
Example of Pacemaker Function:
- Normal heartbeat.
- If the heart pauses, the pacemaker senses the delay.
- Pacemaker sends an impulse to maintain the heartbeat.
- Important Things to Know Before Implantation
- Safety: A pacemaker won’t prolong your life, but it will prevent issues like fainting or dizziness, reducing the risk of falls.
- Improved Quality of Life: Many patients feel more energetic and have better stamina after getting a pacemaker.
- Doesn’t Fix Atrial Fibrillation: If you have atrial fibrillation, you’ll still need to take blood thinners.
- Lifestyle: Your lifestyle won’t change much. In fact, many patients feel better and are able to increase their activity levels.
When Do You Need a Pacemaker?
You may need a pacemaker if you experience:
- Slow heart rate (bradycardia) or pauses longer than 3 seconds
- Fainting or dizziness
- Fatigue, chest pain, or shortness of breath
- Palpitations or decreased stamina
How Does a Pacemaker Work?
- Pacing: If your heart beats too slowly (bradycardia), the pacemaker sends electrical impulses to stimulate the heart to beat faster.
- Sensing: The pacemaker monitors your heart’s activity. When it detects a normal heartbeat, it stays inactive. If it senses a problem, it steps in and sends an impulse to regulate your heart rate.

What to Expect the Day Before Surgery
Medication Instructions:
- Hold blood thinners: Stop Eliquis, Xarelto, or Pradaxa 3 days before surgery. Stop Coumadin until your INR is less than 1.5.
- Stop metformin: Hold for 2 days before surgery. If you take insulin, don’t take your morning dose.
Hospital Instructions:
- The hospital will call you the night before with surgery details.
- No food or drink after midnight before surgery. Take your regular medications with a small sip of water (except blood thinners and metformin).
Preparation:
- Clean your chest with Hibiclens Antiseptic Cleanser the night before and the morning of surgery.
- If allergic to iodine, follow your doctor’s specific instructions.
How is a Pacemaker Implanted?
- The procedure lasts 1-2 hours.
- You’ll receive a sedative, but not general anesthesia.You might be awake, but you won’t feel pain.
- The surgeon makes a small incision under the collarbone and uses X-ray guidance to place wires (leads) into the right ventricle and right atrium of your heart.
- The leads are connected to a generator (the pacemaker’s battery), which is placed under your skin.
PACEMAKER IMPLANT – POST PROCEDURE INSTRUCTIONS
After implant, you may go home the same day, or may stay overnight, depending on your age and other medical conditions
A preventive antibiotic will be prescribed for the next 5 days.
You will be given an ID card that contains information about your pacemaker. You will receive instructions about remote monitoring of your pacemaker at the first visit.
How do I take care of my incision site?
- Keep area with dressing clean and dry for 3 days after your procedure (sponge bath).
- After 3 days you may remove the dressing and shower. The steri strips may fall off; if they don’t, you may peel them away when wet, during showering.
- Avoid spraying water directly on incision while showering in the first 4 weeks
- Pat the incision site dry with a clean towel.
What are my activities instructions?
- Do not lift any objects weighing more than 15 pounds with your affected arm until the wound check in 7-10 days after your procedure.
- Do not raise your arm on the incision side above shoulder level or stretch your arm behind your back for 4 weeks. This gives the leads a chance to secure the proper position and avoid pulling them off
- No driving for 4 weeks. Avoid friction on the incision by the belt.
When you should call Doctor
- Hiccups that won’t stop
- Redness, severe swelling, drainage, worsening pain, bleeding, or warmth at the incision site
- If your pacemaker generator feels loose or wiggling in the pocket under the skin
Potential Complications
- Infection at the implant site
- Allergic reactions to the dye or anesthesia
- Bleeding or bruising at the incision site
- Rare complications: collapsed lung or heart perforation
- Lead dislodgement, which may require a second procedure
After the Pacemaker Implant
Many patients feel that their lack of energy or shortness of breath before the procedure was due to aging. After the pacemaker is implanted, they are often pleasantly surprised to feel more energetic and return to their normal activities with improved stamina.
Leaving a normal life with a pacemaker
It’s unlikely that your pacemaker would stop working properly because of electrical interference. Still, you’ll need to take a few precautions:
- Cellphones. It’s safe to talk on a cellphone but avoid placing your cellphone directly over your pacemaker implantation site.
- Security systems. Passing through an airport metal detector won’t interfere with your pacemaker, although the metal in it may sound the alarm. To avoid potential problems, carry an ID card stating that you have a pacemaker.
- Medical equipment. If a doctor is considering any medical procedure that involves intensive exposure to electromagnetic energy, tell him or her that you have a pacemaker. Such procedures include magnetic resonance imaging, therapeutic radiation for cancer treatment and shock wave lithotripsy, which uses shock waves to break up large kidney stones or gallstones.
- If you’re having surgery, a procedure to control bleeding (electrocautery) also can interfere with pacemaker function.
- Power-generating equipment. Stand at least 2 feet (60 centimeters) from welding equipment, high-voltage transformers or motor-generator systems.
- Cellphones. It’s safe to talk on a cellphone but avoid placing your cellphone directly over your pacemaker implantation site when the phone is turned on. Although unlikely, your pacemaker could misinterpret the cellphone signal as a heartbeat and withhold pacing.
- Generally, microwave ovens, computers, VCRs, and garage door openers are all safe to use.