MALE MENOPAUSE AND HEART

Hormone changes due to aging occur in both men in women triggering a variety of confusing symptoms and mimicking heart disease. Male menopause, andropause or commonly “midlife crisis” is a more gradual process with a steady decline in sex hormones over years, compared to a sudden drop in these hormones in women- which accounts for a more dramatic picture of menopause in females
Nevertheless, andropause can lead to bothersome symptoms and anxiety of not finding a cause or cure, since most tests would be normal expect for low level of testosterone. Testosterone levels gradually decline throughout adulthood — about 1 percent a year after age 30 on average.
Many times, patients end up in a cardiology office with symptoms derived from andropause: shortness of breath, tiredness, palpitations, vague chest pains, elevated blood pressure.
Symptoms due to male menopause
1. Sleep pattern changes: insomnia, or increased sleepiness, leading to fatigue, palpitations and elevated blood pressure
2. Physical changes: increased body fat, reduced muscle bulk and strength, hot flashes, less energy. These changes may resemble heart disease, with shortness of breath, palpitations, increasing weight (which alone may increase the risk of real heart disease) , developing obstructive sleep apnea . Loss of body hair may appear
3.Changes in sexual function: reduced sexual desire, erectile dysfunction, smaller testicles. Understanding these changes as normal age-related process will eliminate anxiety and will lead you to healthy ways to overcome and adapt
4. Emotional changes: sadness, depression, trouble concentrating or remembering things, leading to a more sedentary life, low confidence. Of note, men don’t always experience depression as feelings of sadness., like women, but more of being unusually tired, anxious or irritable.
Conditions that lower testosterone level
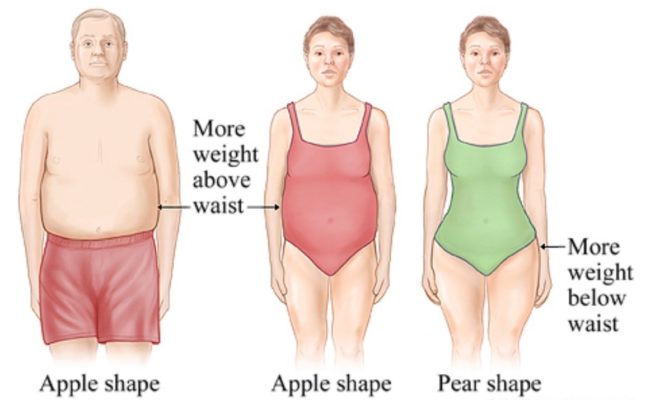
• Obesity, mostly belly fat distribution
• Metabolic syndrome
• High blood pressure
• Diabetes
• High cholesterol levels
• Obstructive sleep apnea
• Use of medications such as antidepressants and narcotic pain medications
• Smoking
• Alcohol abuse
Treatment of male menopause
Treating male menopause with testosterone replacement therapy is controversial.
For some men, with clearly low testosterone levels, testosterone therapy may be beneficial. For others, the benefits aren’t clear and there are possible risks.
The healthiest way to improve testosterone level is to address first all other factors that lowers it
Blood pressure less than 120/70
Diabetes with HbA1C < 6
Obstructive sleep apnea
Obesity – metabolism lowers with age, then you may need to eat less and exercise more to maintain an adequate body weight. Avoid carbohydrates,
Be aware of belly fat distribution – or “apple shape” which triggers metabolic syndrome and low testosterone levels.
Smoking cessation. Decrease alcohol consumption. One small drink a day which is acceptable at this age may be already too much in the face of menopause.Avoid beer or sweetened drinks.Switch your diet to protein based instead of carbohydrates. (will help with muscle waste and with weight maintenance
Be wary of Herbal supplements: not safe for aging-related low testosterone. Some supplements might even be dangerous. Long-term use of DHEA, for example, has no proven benefits and might increase the risk of prostate cancer.
Erectile dysfunction pills are safe and effective if prescribed by a physician. ED drugs available in the United States include Sildenafil (Viagra), Avanafil (Stendra), Tadalafil (Cialis) and Vardenafil (Levitra). There is also a fast-dissolving form of Levitra, called Staxyn, that you put under your tongue. Cialis is FDA-approved for use daily in a dose of 2.5 or 5 milligrams. This helps to induce erections on demand and relieves urinary problems, that result from an enlarged prostate. How the ED pills work?ED drugs produce an erection sufficient for intercourse in about 70% of men. The drugs start working within 15 to 60 minutes Viagra and Levitra will not work if you take them after a meal, which blocks their absorption.Cialis and Stendra do not interact with food this way. The onset time determines how soon you can engage in intercourse.How to use ED pills properly These drugs improve blood supply to the penis. However, they should be combined with sexual stimulation in order to achieve an erection sufficient to initiate and complete intercourse. The drugs don’t work well without sexual stimulation. Dr Liou, chief of urology at Harvard-affiliated Cambridge Health Alliance in Boston, says: “During the time after taking the pill you need to be with your partner and have foreplay, “Don’t take it, do the taxes or the dishes, and then meet at the bedroom thinking you’ll be ready to go. It’s not like that.” How long do ED pills last? The duration of action range from four hours to more than a day (for Cialis in the higher doses). Each dose should be sufficient to provide a full cycle of intercourse, from erection to climax. Quoting Dr. Liou“Will it last through another cycle? It’s not guaranteed,”. To have sex more than once a day, Cialis is your best bet.”
What are the side effects of ED pills?
• headache, flushing, upset stomach, nasal congestion, urinary tract infections, vision problems, diarrhea, dizziness, and rash.
• an erection that lasts four hours or more needs an immediate visit to a hospital or risk permanent damage.
• do not take them with cardiac drugs called nitrates because it could cause a dangerous drop in blood pressure
• be wary of combining them with alpha blockers, – commonly prescribed for prostate problems. The combination can lower blood pressure, so it’s wise to take the two drugs at least four hours apart. From the safest alpha blocker prostate drug is Tamsulosin (Flomax), which affects blood pressure less. While medical community is still debating whether or not men really do go through menopause, there is enough scientific evidence that decreased testosterone starting around 50 is causing real symptoms.
As a cardiologist, I encourage a full heart screening after this age; but if all tests are normal it’s time to acknowledge “male menopause “and treat it accordingly
References:
https://www.webmd.com/men/guide/male-menopause https://www.health.harvard.edu/mens/which-drug-for-erectile-dysfunction
Courtesy: http://womensnewlookandhealthin21stcentury.com/