Women and Heart Disease
Gender bias in understanding, diagnosis, and treatment.
IRINA STAICU, MD, RPVI, ABVLM Diplomat, NUCLEAR CARDI0LOGY DIPLOMAT
“The community has viewed women health almost with a “bikini” approach, looking essentially at breast and reproductive system, ignoring the rest of the women as part of the women’s health “-Nannette Wagner, MD
Screening process allows early recognition of cancers, improving early detection and cure. Women education about mammograms and pap smears led to improved survival.
COLUMBUS, Ohio – A new scientific statement issued today by the American Heart Association underscores knowledge gaps that remain when it comes to women and heart attacks, and outlines the priority steps needed to better understand and treat heart disease in women.
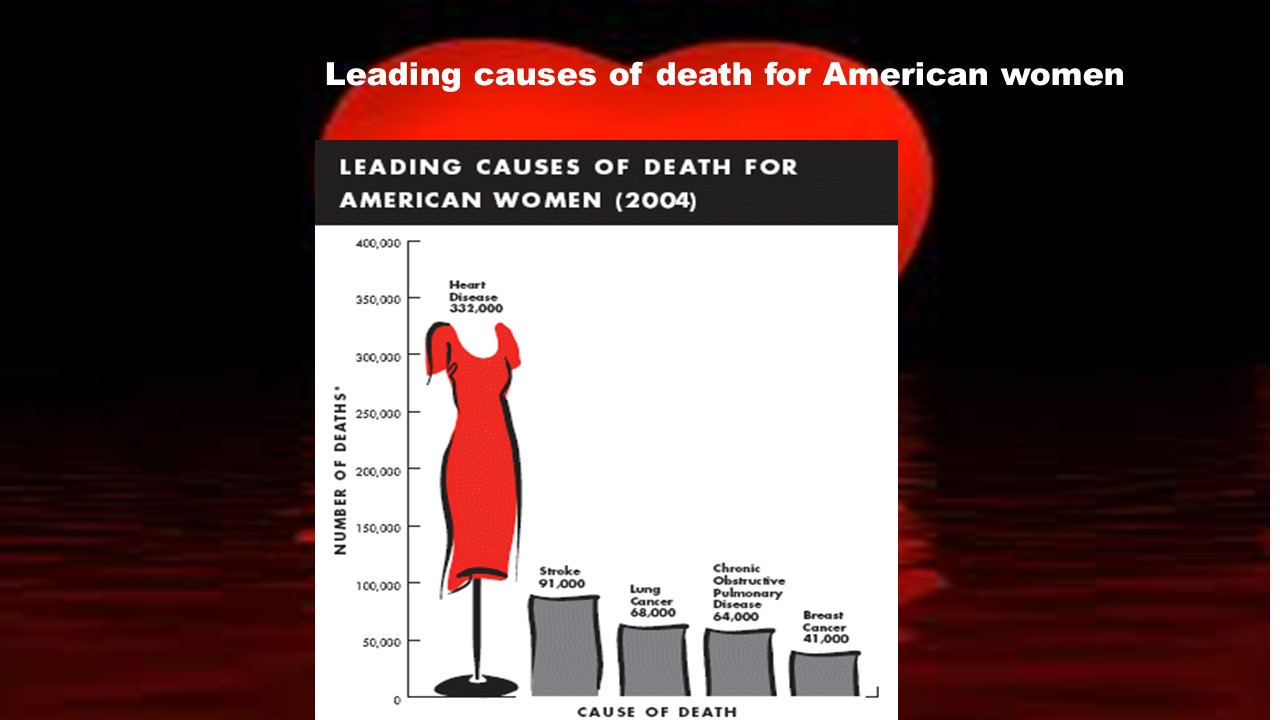
Breast cancer vs. Heart Disease
- For every woman that dies from breast cancer there are six that die from heart disease
- Younger women are twice as likely to die from a heart attack than younger men
- There is higher mortality risk in younger vs. older women
Over 8,000,000 American women live with heart disease
- Between the ages of 45 and 64, one in nine women has some form of heart disease
- Above the age of 65 one in three women has some form of heart disease
- Heart disease may not be recognized, and symptoms may be “blamed on aging”
Why heart disease in women is different
- Smaller heart arteries
- Aspirin to prevent heart attack may have different benefits in women than men
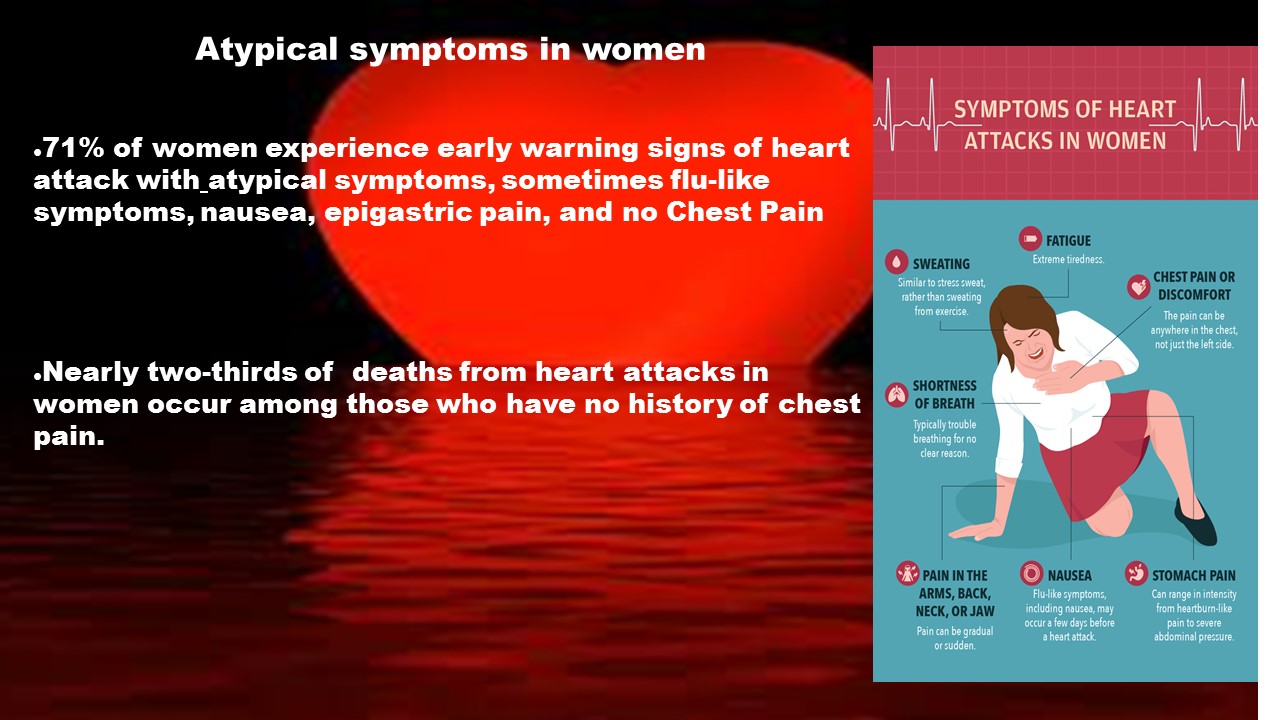
- Atypical symptoms are hard to be recognized: 71% of women experience early warning signs of heart attack with atypical symptoms, sometimes flu-like symptoms, nausea, epigastric pain, and no Chest Pain. Nearly two-thirds of deaths from heart attacks in women occur among those who have no history of chest pain.
- Breast cancer therapy increases the risk of heart attack
- Different response to known heart attack treatments
- Women are more likely to delay treatment in emergency care
- Metabolic syndrome is more common in women
- Heart testing leads to more false results in women than men
Focus on:
- Risk factors recognition and correction
- New non-invasive tests that help in diagnosing of CAD in women
- Aggressive risk factor modification and early recognition of the disease
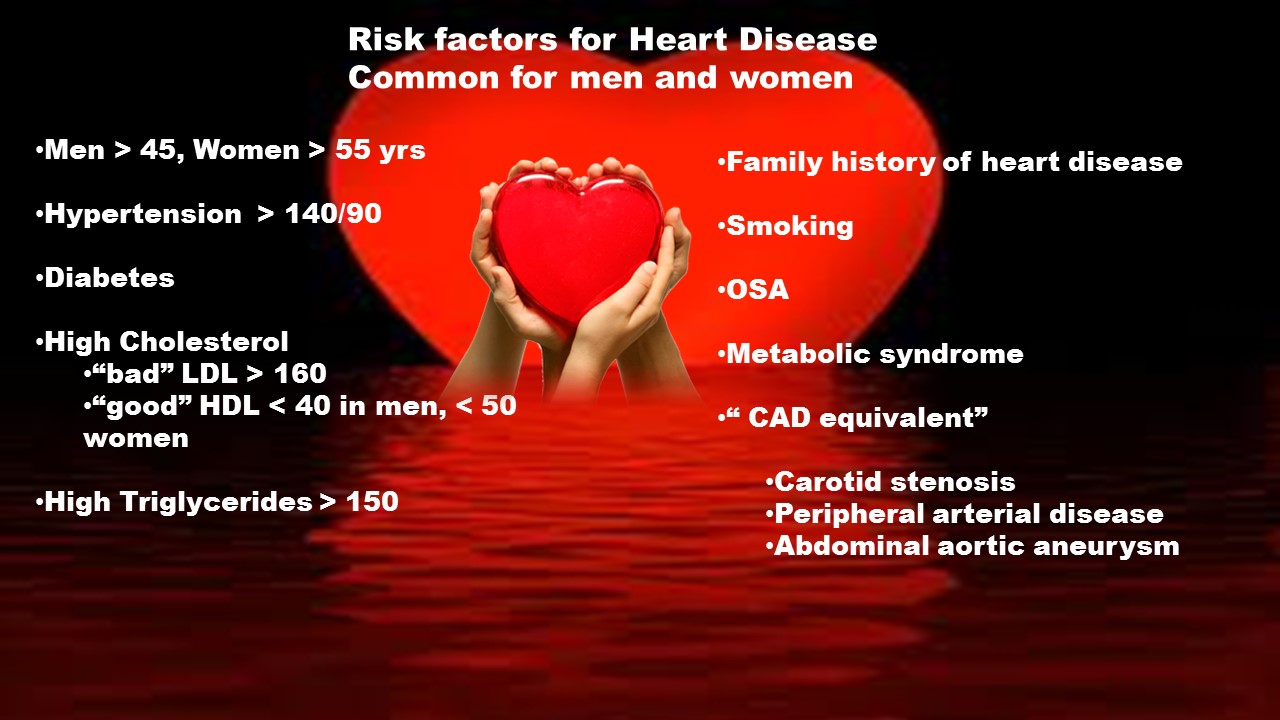
Risk factors for Heart Disease Common for men and women
- Men > 45, Women > 55 yrs.
- Hypertension > 140/90
- Diabetes
- High Cholesterol
- “bad” LDL > 160
- “good” HDL < 40 in men, < 50 women
- High Triglycerides > 150
- Family history of heart disease
- Smoking
- OSA
- Metabolic syndrome
- “CAD equivalent” Carotid stenosis, Peripheral arterial disease, Abdominal aortic aneurysm
Specific Risk factors for Heart Disease in Women
- Anemia
- Early menopause
- Chronic Inflammatory states
- Polycystic ovary
- Rheumatoid arthritis
- Lupus
- Kidney disease
- Thyroid disease
- Low bone density
- Cancer and history of radiation or chemotherapy
- Psycho-social factors
Cardio-Oncology: How cancer affects heart
Chemotherapy and radiation therapy increases the risk of HD.
The risk remains high years after cancer resolution.
Cardiac monitoring decreases the risk of HD and complications of cancer treatment
Today cancer patient may become tomorrow heart patient, without early recognition and treatment
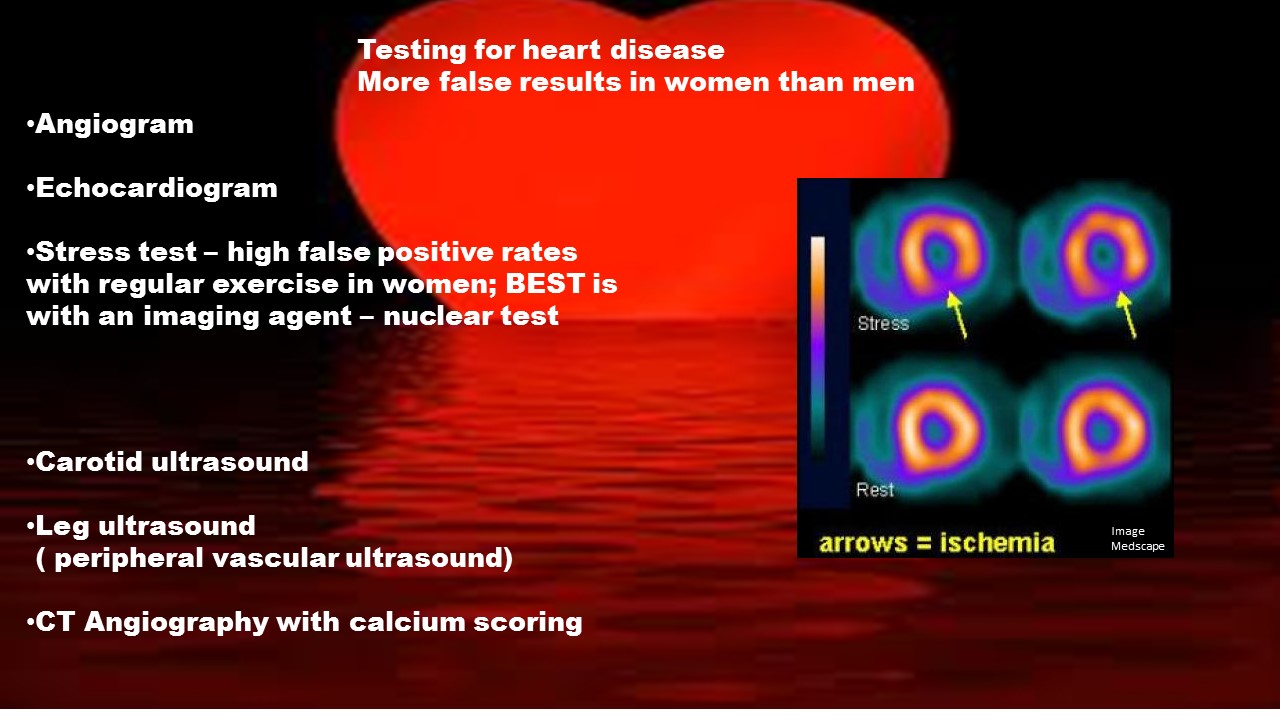
Testing for heart disease:
- Angiogram
- Echocardiogram
- Stress test – high false positive rates with regular exercise in women; BEST is with an imaging agent – nuclear test
- Carotid ultrasound
- Leg ultrasound (peripheral vascular ultrasound)
- CT Angiography with calcium scoring
Where do we go from here?
- Acknowledge
- High incidence of HD – Number 1 Killer in women
- Atypical symptoms
- Challenges in diagnosing HD in women
- Worse outcome in women than men
- Recognize
- Unique Risk factors in women
- The importance of HD prevention
- Be knowledgeable and your own advocate